BIOEQUIVALENCE: Its type and method of studying bioequivalence
BIOEQUIVALENCE:
It‘s commonly observed that there are several formulations of the same drug, in the same dose, in similar dosage form and meant to be given by the same route. in order to ensure clinical performance of such drug products, bioequivalence studies should be performed.
TYPES OF EQUIVALENCE
- Chemical Equivalence:
- When 2 or more drug products contain the same labeled chemical substance as an active ingredient in the same amount.
- Pharmaceutical Equivalence:
- When two or more drug products are identical in strength, quality, purity, content uniformity, disintegration and dissolution characteristics; they may however differ in excipients.
- Bioequivalence:
- A relative term which denotes that the drug substance in two or more dosage forms, reaches the systemic circulation at the same relative rate and to the same relative extent i.e., their plasma concentration time profiles will be identical without significant statistical difference.
- Therapeutic Equivalence:
- When two or more drug products that contain the same therapeutically active ingredient, elicit identical pharmacologic response and can control the disease to the same extent.
- It does not encompass a comparison of different therapeutic agent used in the same condition.
- The FDA considers drug products to be therapeutically equivalent if they meet the following criteria:
- 1. Approved as safe and effective.
- 2. Pharmaceutically equivalent
- 3. Bioequivalent
- 4. Adequately labeled
- 5. Manufactured in compliance with cGMP.
- Although, they may differ in characteristics like, Shape, release mechanism, excipients, packaging, minor aspects of labeling (like the presence of specific pharmacokinetic information), expiration date/ time, etc.
- The FDA believes that products classified as therapeutically equivalent can be substituted with the same expectation that the substituted product will produce the same clinical effect and safety profile as the prescribed product.
- Clinical Equivalence:
- When the same drug from 2 or more dosage forms gives identical in vivo effects as measured by pharmacological response or by control over a symptom or a disease.
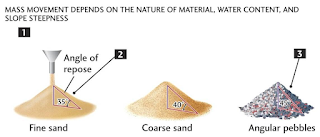
- During the development of a drug product, certain biopharmaceutical properties of the active drug substance or the formulation of the drug product may indicate that the drug may have variable bioavailability and/or a bioequivalence problem. Some of these biopharmaceutic properties include:
- The active drug ingredient has low solubility in water (eg, less than 5 mg/mL).
- The dissolution rate of one or more such products is slow (eg, less than 50% in 30 minutes when tested with a general method specified by the FDA).
- The particle size and/or surface area of the active drug ingredient is critical in determining its bioavailability.
- Certain structural forms of the active drug ingredient (eg, polymorphic forms, solvates, complexes, and crystal modifications) dissolve poorly, thus affecting absorption.
- Drug products that have a high ratio of excipients to active ingredients (eg, greater than 5:1).
- Specific inactive ingredients (eg, hydrophilic or hydrophobic excipients and lubricants) either may be required for absorption of the active drug ingredient or therapeutic moiety or may interfere with such absorption.
- The active drug ingredient, therapeutic moiety, or its precursor is absorbed in large part in a particular segment of the GI tract or is absorbed from a localized site.
- The degree of absorption of the active drug ingredient, therapeutic moiety, or its precursor is poor (eg, less than 50%, ordinarily in comparison to an intravenous dose), even when it is administered in pure form (eg, in solution).
- There is rapid metabolism of the therapeutic moiety in the intestinal wall or liver during the absorption process (first-order metabolism), so that the rate of absorption is unusually important in the therapeutic effect and/or toxicity of the drug product.
- The therapeutic moiety is rapidly metabolized or excreted, so that rapid dissolution and absorption are required for effectiveness.
- The active drug ingredient or therapeutic moiety is unstable in specific portions of the GI tract and requires special coatings or formulations (eg, buffers, enteric coatings, and film coatings) to ensure adequate absorption.
- The drug product is subject to dose-dependent kinetics in or near the therapeutic range, and the rate and extent of absorption are important to bioequivalence.
A. IN VIVO BIOEQUIVALENCE STUDY
- It requires determination of relative bioavailability after administration of a single dose of test and reference formulations by the same route, in equal doses, but at different times.
- The reference product is generally a previously approved product, usually a innovator‘s product or some suitable reference standard.
- The study is performed in fasting, young, healthy, adult male volunteers to assure homogeneity in the population & to spare the patients, elderly or pregnant women from rigors of such a clinical investigation.
1. PARALLEL GROUP DESIGN:
- In a parallel group design, subjects are divided randomly into groups, each group receiving one treatment randomly.
- Here number of groups is same as number of treatments to be compared.
- Each subject receives only one treatment.
- Arrangements in which each subject receives two or more different treatments on successive occasions, are known as cross over designs.
- In this design, the number of treatments is same as the number of periods.
- This design can be used with any number of treatments, subjects to the restriction that the number of subjects must be a multiple of the number of treatments.
1. LATIN SQUARE CROSS OVER DESIGN: In which
- Each formulation is administered just once to each subject & once in each study period, &
- Unlike parallel design, all the subjects do not receive the same formulation at the same time; in a given study period, they are administered different formulations.
- An example of the Latin square cross- over design for a bioequivalence study in human volunteers is given in following table:-
- Examples of Latin-square crossover designs for a bioequivalence study in human volunteers, comparing three different drug formulations (A, B, C).
- The Latin-square design plans the clinical trial so that each subject receives each drug product only once, with adequate time between medications for the elimination of the drug from the body.
- In this design, each subject is his own control, and subject-to-subject variation is reduced. Moreover, variation due to sequence, period, and treatment (formulation) are reduced, so that all patients do not receive the same drug product on the same day and in the same order.
- Possible carryover effects from any particular drug product are minimized by changing the sequence or order in which the drug products are given to the subject.
- Thus, drug product B may be followed by drug product A, D, or C.
- After each subject receives a drug product, blood samples are collected at appropriate time intervals so that a valid blood drug level–time curve is obtained. The time intervals should be spaced so that the peak blood concentration, the total area under the curve, and the absorption and elimination phases of the curve may be well described.
2. REPLICATED CROSS OVER DESIGN
Replicated crossover designs are used for the determination of individual bioequivalence, to estimate within-subject variance for both the Test and Reference drug products, and to provide an estimate of the subject-by-formulation interaction variance. Generally, a four-period, two-sequence, two-formulation design is recommended by the FDA.
The same reference and the same test are each given twice to the same subject. Other sequences are possible. In this design, Reference-to-Reference and Test-to-Test comparisons may also be made.
Advantages of Cross over design:
- Minimize intersubject variability in plasma drug level.
- Minimize intrasubject variability → affecting bioavailability of a subsequently administered product.
- Minimize variation due to time effect.
- Make it more possible to focus more on formulation variables which is the key to success for any bioequivalence study.
- Takes long time since appropriate washout period between 2 administrations is essential.
- Time may be longer if the drug has t1/2 long.
- When the no. of formulations to be tested are more, the study becomes more difficult and subject dropout rate may increase.
- This can be overcome by use of a balanced incomplete design in which a subject receives no more that two formulations.
EVALUATION OF THE DATA:
Analytical Method:
- The analytical method for measurement of the drug must be validated for accuracy, precision, sensitivity, and specificity.
- The use of more than one analytical method during a bioequivalence study may not be valid, because different methods may yield different values.
- Data should be presented in both tabulated and graphic form for evaluation.
- The plasma drug concentration–time curve for each drug product and each subject should be available.
- For single-dose studies, including a fasting study or a food intervention study, the pharmacokinetic analyses include calculation for each subject of the area under the curve to the last quantifiable concentration (AUC0–t) and to infinity (AUC0–∞), T max, and C max.
- Additionally, the elimination rate constant, k, the elimination half-life, t 1/2, and other parameters may be estimated.
- For multiple-dose studies, pharmacokinetic analysis includes calculation for each subject of the steady-state area under the curve, (AUC0–t), T max, C min, C max, and the percent fluctuation [100 x (C max – C min)/C min]. Proper statistical evaluation should be performed on the estimated pharmacokinetic parameters.
- Bioequivalence is generally determined using a comparison of population averages of a bioequivalence metric, such as AUC and C max.
- This approach, termed average bioequivalence, involves the calculation of a 90% confidence interval for the ratio of averages (population geometric means) of the bioequivalence metrics for the Test and Reference drug products.
- To establish bioequivalence, the calculated confidence interval should fall within a prescribed bioequivalence limit, usually, 80–125% for the ratio of the product averages. Standard crossover design studies are used to obtain the data.
- Another approach proposed by the FDA and others is termed individual bioequivalence. Individual bioequivalence requires a replicate crossover design, and estimates within-subject variability for the Test and Reference drug products, as well as subject-by-formulation interaction.
- Presently, only average bioequivalence estimates are used to establish bioequivalence of generic drug products.
- To prove bioequivalence, there must be no statistical difference between the bioavailability of the Test product and the Reference product. Several statistical approaches are used to compare the bioavailability of drug from the test dosage form to the bioavailability of the drug from the reference dosage form.
- Many statistical approaches (parametric tests) assume that the data are distributed according to a normal distribution or "bell-shaped curve" . The distribution of many biological parameters such as C max and AUC have a longer right tail than would be observed in a normal distribution.
- Moreover, the true distribution of these biological parameters may be difficult to ascertain because of the small number of subjects used in a bioequivalence study. The distribution of data that has been transformed to log values resembles more closely a normal distribution compared to the distribution of non-log-transformed data.
- Therefore, log transformation of the bioavailability data (eg, C max, AUC) is performed before statistical data evaluation for bioequivalence determination.
- An analysis of variance (ANOVA) is a statistical procedure used to test the data for differences within and between treatment and control groups.
- A bioequivalent product should produce no significant difference in all pharmacokinetic parameters tested.
- The parameters tested usually include AUC0–t, AUC0–∞, t max, and C max obtained for each treatment or dosage form. Other metrics of bioavailability have also been used to compare the bioequivalence of two or more formulations.
- The ANOVA may evaluate variability in subjects, treatment groups, study period, formulation, and other variables, depending on the study design. If the variability in the data is large, the difference in means for each pharmacokinetic parameter, such as AUC, may be masked, and the investigator might erroneously conclude that the two drug products are bioequivalent.
- A statistical difference between the pharmacokinetic parameters obtained from two or more drug products is considered statistically significant if there is a probability of less than 1 in 20 times or 0.05 probability (p ≤0.05) that these results would have happened on the basis of chance alone. The probability, p, is used to indicate the level of statistical significance. If p < 0.05, the differences between the two drug products are not considered statistically significant.
- To reduce the possibility of failing to detect small differences between the test products, a power test is performed to calculate the probability that the conclusion of the ANOVA is valid. The power of the test will depend on the sample size, variability of the data, and desired level of significance. Usually the power is set at 0.80 with a β= 0.2 and a level of significance of 0.05. The higher the power, the more sensitive the test and the greater the probability that the conclusion of the ANOVA is valid.
- The two one-sided tests procedure is also referred to as the confidence interval approach. This statistical method is used to demonstrate if the bioavailability of the drug from the Test formulation is too low or high in comparison to that of the Reference product. The objective of the approach is to determine if there are large differences (ie, greater than 20%) between the mean parameters.
- The 90% confidence limits are estimated for the sample means. The interval estimate is based on a Student's t distribution of the data.
- In this test, presently required by the FDA, a 90% confidence interval about the ratio of means of the two drug products must be within ±20% for measurement of the rate and extent of drug bioavailability. For most drugs, up to a 20% difference in AUC or C max between two formulations would have no clinical significance.
- The lower 90% confidence interval for the ratio of means cannot be less than 0.80, and the upper 90% confidence interval for the ratio of the means cannot be greater than 1.20. When log-transformed data are used, the 90% confidence interval is set at 80– 125%. These confidence limits have also been termed the bioequivalence interval . The 90% confidence interval is a function of sample size and study variability, including inter- and intrasubject variability.
- For a single-dose, fasting study, an analysis of variance (ANOVA) is usually performed on the log-transformed AUC and C max values. There should be no statistical differences between the mean AUC and C max parameters for the Test (generic) and Reference drug products.
- In addition, the 90% confidence intervals about the ratio of the means for AUC and C max values of the Test drug product should not be less than 0.80 (80%) nor greater than 1.25 (125%) of that of the Reference product based on log-transformed data.
- In following circumstances equivalence may be assessed by the use of in vitro dissolution testing:
- Drugs for which the applicant provide data to substantiate all of the following:
- Highest dose strength is soluble in 250ml of an aqueous media over the pH range of 1-7.5 at 37*C.
- At least 90% of the administered oral dose is absorbed on mass balance determination or in comparison to an intravenous reference dose.
- Speed of dissolution as demonstrated by more than 80% dissolution within 15 minutes at 37*C using IP apparatus 1, at 50 rpm or IP apparatus 2, at 100rpm in a volume of 900 ml or less in each of the following media:
- 0.1 N hydrochloric acid or artificial gastric juice (without enzymes)
- A pH 4.5 buffer
- A pH 6.8 buffer or artificial intestinal juice (without enzyme)
- Different strength of the drug manufactured by the same manufacturer, where all of the following criteria are fulfilled:
- The qualitative composition between the strengths is essentially the same;
- The ratio of active ingredients and excipients between the strength is essentially the same or in the case of small strength, the ratio between the excipients is the same;
- The method of manufacture is essentially the same;
- An appropriate equivalence study has been performed on at least one of the strength of the formulation (usually the highest strength unless a lower strength is chosen for reasons of safety); and
- In case of systemic availability-pharmacokinetics have been shown to be linear over the therapeutic dose range.
- In vitro dissolution testing may also be suitable to confirm unchanged product quality and performance characteristics with minor formulation or manufacturing changes after approval.
- Studies in healthy volunteers of patients using pharmacodynamic parameters may be used for establishing equivalence between two pharmaceutical products. These studies may become necessary
- If quantitative analysis of the drug and/or metabolite(s) in plasma or urine cannot be made with sufficient accuracy and sensitivity.
- If measurement of drug concentrations cannot be used as surrogate endpoints for the demonstration of efficacy and safety of the particular pharmaceutical product e.g. topical products without an intended absorption of the drug into the systemic circulation.
It is carried out when
- The plasma concentration time-profile date may not be suitable to assess equivalence between two formulations.
- Pharmacodynamic studies cannot be performed because of lack of meaningful pharmacodynamic parameters, which can be measured.
- Pharmacodynamic and pharmacokinetic studies are not feasible.
- The use of stereoselective method in bioequivalence studies is an important goal to be realized in future.
- Stereoselective methods should be used in two situation:
- When there is high first pass metabolism of the active enantiomer (eutomer) → suggests that both total and eutomer concentrations should be measured.
- When there is low first pass metabolism of the eutomer, each enantiomer should be measured separately.
- In all other cases, nonstereoselective methods should suffice.
The impact of stereoisomerism in a bioequivalence study on two formulations of doxepin
- A bioequivalence study was carried out on two formulations of doxepin containing 15% of the active cis isomer and 85% of the less active trans isomer..The 90% confidence intervals (In AUClast, In Cmax and In Cmax/AUClast) for Ndesmethyldoxepin fell entirely within bioequivalence li whether stereoselective or non-stereoselective data were analyzed. Thus the results of this study did not support arguments in favor of the use of stereoselective methods in bioequivalence studies (Ref: European journal of pharmaceutical sciences,Vol 4, issue3, may1996, pg:133-138)
- For controlled release products administered once a day, a three way cross over study comparing the test formulation with an approved controlled release drug product under fasting conditions is conducted to ensure controlled release nature of the test product as well as the absence of dose dumping.
- Following are the cases where bioequivalence studies are not necessary:
- An aqueous solution for parenteral use
- A solution for oral use
- A gas
- A powder for reconstitution as a solution for oral or parenteral use
- An otic or ophthalmic solution
- A topical aqueous solution
- An inhalation product or nasal spray as an aqueous solution.
REFERENCES:
1. Applied Biopharmaceutics and Pharmacokinetics,5th Edition By Leon Shargel
2. Biopharmaceutics and pharmacokinetics – A treatise by – D.M. Brahmankar
3. Guidelines for bioavailability and bioequivalence studies By Central Drugs Standard Control Organization
4. Note for guidance on the investigation of Bioavailability and Bioequivalence By Committee for Proprietary Medicinal Products(CPMP)
5. Encyclopedia of pharmaceutical technology; Vol – 1
6. Remington: The Science and Practice of Pharmacy; Vol – 1
7. Pharmacokinetics; Dekker series; Vol 33
8. Bioavailability and Bioequivalence: General Concepts and Overview- Rich Bergstrom, Ph.D., Jennifer Witcher, Ph.D.
9. http://www.fda.gov/cder/ob/docs/preface/ecpreface.htm.
10. http://www.fda.gov/cder/ob/default.htm.
11. Journal of Food and Drug Analysis. 1994.Vol 2(Number3) : Pg155-160
12. International journal of p‘ceutics ,Vol86, issue2-3, 26 oct 1992, pg 123-130
13. European journal of pharmaceutical sciences,Vol 4, issue3, may1996, pg:133-138)
14. http://jclinpharm.highwire.org/cgi/content/abstract/46/3/282
15. International journal of pharmaceutics,Vol.304,issues1-2, 4Nov,2005,pg63-71
16. Contraception,Vol.40,issue 5,nov1989,pg 581-590
17. Current Therapeutic Research,Vol64, issue9, Nov-Dec 2003,pg 685-696
18. CA,Vol-151,NO 12,Sept21,2009 ,pgno 1525, 272547e
19. CA, Vol-151, no13, sept28,2009 ,pg2100, 297392p
20. CA, Vol-151, no13, sept28,2009 ,pg2100, 297392q
21. JPS, Vol98, NO1,Jan 2009, pg319





Comments
Post a Comment